No, Statins Do NOT Prevent Dementia and Alzheimer's Disease.
Biased studies conducted by pharma-funded researchers are not proof of anything.
Many of you will be familiar with Dr Peter McCullough, the US cardiologist who has prominently - and admirably - spoken out against the toxic COVID 'vaccines.'
He's also co-authored numerous published papers on 'vaccine' harms with other notable skeptics, including Stephanie Seneff, Jessica Rose, Megan Redshaw and Steve Kirsch.
All of which leaves me puzzled by a recent Substack post in which Dr McCullough praises another class of toxic drugs. His post makes the audacious - and false - claim that cholesterol-lowering statin drugs reduce the risk of dementia and Alzheimers Disease.
He bases this untenable claim entirely upon a 2022 meta-analysis of epidemiological studies by Italian researchers - two of whom have extensive ties to pharma companies, including cholesterol-lowering drug manufacturers like Pfizer, Merck, Amgen, Servier and Sanofi-Regeneron.
McCullough's post is not just disappointing - it's dangerous.
McCullough has built up a large following, with almost 1 million followers on Twitter and 104,000 subscribers on Substack. He has been a regular fixture on alternative media channels and COVID documentaries, and even appeared on the world’s most popular podcast, The Joe Rogan Experience.
Which means he has a lot of admiring fans who are being fed a blatant falsehood: The absurd claim that statin drugs are good for brain health, to the point where they lower the risk of dementia and Alzheimer’s Disease.
Read my lips:
Statin drugs do NOT lower the risk of dementia and Alzheimer’s Disease.
To the contrary, they are toxic garbage that should never have been allowed to market - just like the mortality-boosting gene therapies being passed off as 'COVID' vaccines.
As is so often the case with uber-absurd claims, it's hard to know where to start with this one.
So let's start with the basics.
Cholesterol and the Mammalian Brain: A 300 Million Year-Old Love Affair
Health authorities have long told us cholesterol is bad. These are the same people who more recently told us getting injected with drugs based on repeatedly-failed mRNA technology was good.
Health authorities, it must be said, are largely full of caca.
The reality is that cholesterol is good for you. It is an integral component of every cell in your body. Without it, you'd collapse into an unsightly pile of bones, hair and mush.
Cholesterol is found in especially high concentrations in the nervous system and in your brain. Even though the central nervous system accounts for only 2.1% of body weight, it contains 23% of the body's cholesterol.
Your brain and nerves thrive on cholesterol. When your CNS is deprived of cholesterol, things start going haywire.
Read the following passage, by Polish scientists with a clue, very carefully:
"Cholesterol is an important structural component of nerve cells, and the brain is the most cholesterol-rich organ, containing about 20% of the total body’s cholesterol. Brain cholesterol exists in two pools: the plasma membranes of neurons and glial cells and the myelin membranes, with the majority (70%) located in the myelin. Cholesterol is the main constituent of cell membranes. In many neurons, it constitutes the myelin sheath providing insulation for the conduction of nerve impulses; therefore, its loss greatly contributes to neurological problems. Cholesterol affects the functioning of brain synapses, and is crucial in production, and secretion of neurotransmitters. Cholesterol and lipid homeostasis are critical for normal brain function, including neuronal repair, membrane remodeling, and plasticity. A link between cholesterol metabolism defects and neurodegenerative disorders is now recognized." (Bold emphasis added).
Everything they've said above is verifiable fact. Cholesterol is a key component of your cells, nerves and brain. Cholesterol is crucial for a healthy nervous system and cognitive function.
Which helps explain why low cholesterol levels have long been associated with an increased risk of depression, suicide and violent death.
Yours truly, along with others like Uffe Ravnskov, the late Duane "Spacedoc" Graveline and Beatrice Golomb, MD, PhD, could have told you this twenty years ago.
In fact, we did.
In a 2004 paper, Dr Golomb and colleagues described six patients presenting with irritability and short temper whilst on statin drugs. In each case these negative personality changes persisted until statin use was discontinued and resolved promptly with drug cessation. Four of the patients resumed statin therapy, and in each case the problems reappeared. Among the manifestations of severe irritability in these patients were homicidal impulses, threats to others, road rage, generation of fear in family members, and damage to property.
The previous year, Psychoneuroendocrinology published a clinical trial involving 120 healthy men with high cholesterol who took twenty milligrams of simvastatin for a twelve week period and a placebo for another twelve weeks; a significant increase in depression scores occurred while the men were taking simvastatin.
A 1992 double-blind, placebo-controlled trial found that healthy young men randomized to receive the popular cholesterol-lowering drug lovastatin (Mevacor) displayed significant deterioration in divided attention (the ability to simultaneously focus on multiple tasks and stimuli), vigilance (the ability to sustain attention) and global performance (a more general assessment of cognitive function). These changes were seen after only three weeks of treatment. The ability to maintain divided attention is essential for tasks such as safe driving.
In 2000, Muldoon et al reported the results of a double-blind, placebo-controlled trial that assessed cognitive function and psychological well-being in healthy adults randomly assigned to receive either lovastatin or a placebo. At the start and at the conclusion of the study, subjects were given a battery of tests assessing attention, psychomotor speed, mental flexibility, working memory, and memory retrieval.
After six-months' month follow-up, the placebo group had improved significantly in all five domains of cognitive function, but the lovastatin group improved only on memory recall tests.
When Muldoon and his team subsequently performed another study, this time using simvastatin, they obtained similar results. Failure to improve on cognitive tests was observed with both ten and forty milligram doses of simvastatin.
Statins: Causing cognitive impairment, depression, homicidal thoughts, road rage and property damage - now here to save you from dementia!
Sure.
So where do Italian researchers get off on making the absurd claim that neurotoxic statin drugs can lower the risk of Alzheimer’s and dementia?
By doing what health authorities and mainstream researchers always do when their agenda is not supported by controlled clinical evidence:
Pretend the clinical research doesn't exist, and instead embrace uncontrolled, confounder-prone slop!
How to Portray a Neurotoxic Drug as Good for Your Brain
The study McCullough cites, Olmastroni et al, was published in the March 2022 issue of European Journal of Preventive Cardiology.
Of the nine listed authors, at least two have received financial largesse from numerous drug companies.
Alberico L. Catapano has received research funding and/or honoraria for advisory boards, consultancy or speaker bureau from Aegerion, Amgen, AstraZeneca, Eli Lilly, Genzyme, Mediolanum, Merck or MSD, Pfizer, Recordati, Rottapharm, SanofiRegeneron, and Sigma-Tau.
Alberto Zambon has received honoraria/expenses from Amgen, Eli Lilly, Abbott-Mylan, Servier, Sanofi-Regeneron, Amryt, Amarin, and Daiichi Sankyo.
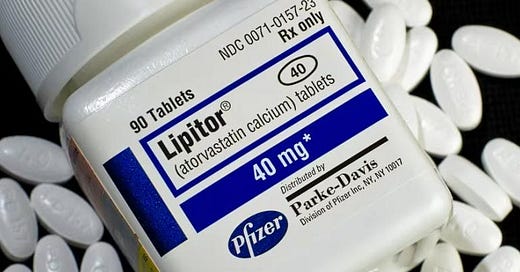
Several of those companies manufacture cholesterol-lowering drugs. Most notably, Pfizer - the same pack of criminals who brought you the Pfizercarditis shot - was responsible for the 'blockbuster' atorvastatin (Lipitor), while Merck's lovastatin (Mevacor) was given FDA approval to become the first commercial statin in 1987. Merck also patented Simvastatin (Zocor) which hit the market five years later.
Their lengthy pharma connections help explain why the researchers blissfully ignored the evidence of harm shown in controlled trials, and instead deferred to confounder-prone epidemiological studies.
My long time readers will already know the difference between randomized, controlled clinical trials and uncontrolled epidemiological studies. For those unfamiliar with these very different modes of research, here's a quick rundown.
Randomized clinical trials (RCTs) involve recruiting a group of subjects, then randomly assigning them to an intervention group or a control group. The randomization helps minimize the effect of confounding variables by producing a fairly even demographic profile between the two groups (i.e. similar average age, similar number of smokers, similar socioeconomic and ethnic mix, and so on). Ideally, these trials are double-blind, which means both researchers and subjects are unaware of who's getting what. This helps removes bias (sometimes it's still possible to tell what a subject is taking by the type of side effects they experience).
Randomized, double-blind clinical trials are considered the gold standard of evidence, and results from such trials are required before new drugs can be approved in the US.
In an epidemiological study, there is no intervention, no randomization, no blinding and an almost infinite array of confounding variables. In prospective or observational epidemiological studies, a bunch of subjects are simply asked to fill out questionnaires and then followed for periods that can last decades. As ridiculous as it sounds, sometimes a single survey at the start is taken as proof of each subject's habits throughout the entire follow-up period.
A case-control study is even less reliable, as it involves past recall. Given that many people struggle to remember what they ate the day before last, it's a sketchy endeavour to rely on people's recall of what they ate or swallowed every day for the last umpteen years.
You've no doubt heard the saying, "association does not equal causation." This is the golden rule when considering the findings of epidemiological studies. They do not and cannot eliminate the effect of confounding variables. They can only detect associations between a variable and an outcome, and even then the strength of those associations needs to be considered in light of the considerable fallibility inherent in human reporting and recall.
Before I discuss the epidemiological tripe Olmastroni et al held up as evidence, let's take a look at what actual double-blind RCTs on the subject revealed.
In 2014, the Cochrane Database of Systematic Reviews - a far more reliable source than researchers getting their palms greased by Big Pharma - published a review titled "Statins for the treatment of dementia."
The researchers scoured scientific databases for studies involving subjects with a probable or possible diagnosis of Alzheimer's disease according to standard clinical criteria, in which a statin or placebo was given for at least six months.
They identified four double-blind RCTs, collectively comprising 1,154 participants with an age range of 50 to 90 years.
The intervention drugs were atorvastatin and simvastatin (two trials each).
The primary outcome in all studies was change in Alzheimer's Disease Assessment Scale - cognitive subscale (ADAS-Cog) from baseline.
When the Cochrane researchers pooled the data, statin use showed no significant benefit on ADAS-Cog score.
All four studies also assessed change in Mini Mental State Examination (MMSE) from baseline. Again, statins showed no significant benefit in MMSE.
In terms of real world changes, there was no significant difference in behaviour, global function or activities of daily living in the statin and placebo groups.
"From these trials, including two large trials," wrote the researchers, "we found no evidence that statins help in the treatment of cognitive decline in dementia."
The Cochrane researchers rated the quality of evidence as high, and assessed risk of bias as low for all four studies.
But hey, who needs high-quality, low-bias RCTs that don't support the agenda of your paymasters, when there are dozens of low-quality, high-bias studies that do, right?
And so Olmastroni et al bissfully ignored the RCTs, and instead scoured the literature for epidemiological studies of the utterly uncontrolled type. They ended up with 38 prospective cohort studies and 8 case–control studies.
The odds ratios of these studies ranged from 0.21 to 1.20 (a ratio lower than 1 represents reduced risk, greater than 1 represents increased risk).
After throwing all this porqueria into their statistical soup bowl, the Italian researchers returned an overall odds ratio of 0.80 for dementia, and 0.68 for Alzheimers. This led McCullough to excitedly claim that statins produce a "Pooled 32% Risk Reduction in Alzheimer's Disease Over a Few Years."
The logical answer to this, of course, nonsense.
We already know from the far higher quality RCT evidence discussed above that the Olmastroni et al findings are simply a statistical fantasy.
We know that statins given to healthy people in RCTs cause harmful cognitive effects.
We know that when statins are given to people with possible or probable dementia, they show no statistically or clinically significant benefit.
So to instead point to a study like that of Olmastroni et al, relying as it did on unreliable epidemiological studies, and claim that it proves statins prevent dementia is terribly misguided at best.
So What Really Caused the Alleged Risk Reductions in Olmastroni et al?
Why did some - not all - epidemiological studies detect a reduced risk of dementia and Alzheimer’s associated with - not caused by - statin use?
Some of you have no doubt heard of the “Healthy Participant Effect.” This is the phenomenon in which health-conscious people tend to volunteer to participate in health studies at a higher rate because, well, health is something that interests them.
The problem is that this can skew the results in a direction that is not really representative of the general population.
A variation of this is the "Healthy Meat Avoider Effect," often seen in Western studies purporting to examine the effect of red meat on cancer or cardiovascular disease. These studies often claim an increased risk for red meat eaters. However, when you look at the demographic data, it becomes clear those who eat the most red meat tend to have the poorest health habits.
Why?
Because Western populations have been bombarded with anti-red meat propaganda for decades now, and so health-conscious people in the West tend to eat less red meat. Their lower cancer or CVD risk stems, not from avoiding red meat, but their overall healthier lifestyles.
In studies of Asian populations, this association vanishes, because those countries have not succumbed to the idiotic anti-meat propaganda of the West.
In fact, a recent study of 175 countries found that red meat was associated with lower mortality risk (I wrote up that study here).
"Yeah," I hear you asking, "but what does all this have to do with statins and dementia?"
Everything.
The studies showing associations between statin use and reduce dementia/Alzheimers risk are confounded by what we can call the "Healthy Statin User Effect."
Let me explain.
In line with the results of the aforementioned experimental studies, there is a wealth of empirical evidence showing those with high cholesterol enjoy a lower risk of neurological, cognitive and psychiatric disorders.
Before statins hit their wholly undeserved peak in popularity, research groups like Steegmans et al and Morgan et al had already found a significant increase in the frequency and severity of depression amongst middle-aged and elderly men with low cholesterol levels when compared to those with higher levels.
Muldoon et al tested over four thousand people aged twenty to fifty-nine, and found that as cholesterol concentrations in males decreased, so too did visuomotor speed. This is one of the qualities that determines whether you react quickly enough in emergency situations to save yourself from permanent extinction. When some a-hole runs a red light and speeds into your direct line of travel, a deficit in reaction time could quite literally mean the difference between getting home safely or ending up on a steel bed with a tag on your toe.
Muldoon and his team found the mean total reaction time of men in the lowest category of blood cholesterol (average 152 mg/dl) was 12.7 milliseconds slower than that of men in the highest category (average 242 mg/dl).
To place these results into better perspective, the difference in reaction time between the highest and lowest cholesterol categories was several times greater than that caused by three decades of aging.
When mortality data during 1993 was obtained for over eleven thousand participants in the 1970-1972 Nutrition Canada Survey, those with a total cholesterol level of less than 4.27 were more than six times as likely to commit suicide as subjects with a cholesterol reading greater than 5.77. These results were adjusted for age and sex, and persisted even after excluding the first five years of follow-up, those who were unemployed, and those who had been treated for depression.
As part of the NHLBI's Twin Study, researchers measured the blood cholesterol of forty-four sets of twins, then followed their cognitive status over the next five years. Among monozygotic twins displaying a discordant decline in a test of information processing speed, the decliners had lower serum cholesterol levels than their non-declining siblings.
Among the Finnish cohort of the infamous Seven Countries Study, 25-year follow-up of 716 men found low serum cholesterol to be a predictor of mental disability.
If you check the dates on the above studies, you'll note they were all published prior to 2000. I deliberately set this cut-off to avoid the confounding effect of statin use, which kicked off in the early 1990s. It wasn't until the 2000s that doctors started handing out these drugs like candy.
One study I'll make an exception for is The Prospective Population Study of Women published in 2010, consisting of 1,462 women without dementia aged 38–60 years and initiated in 1968–1969 in Gothenburg, Sweden. Follow-ups were conducted in 1974–1975, 1980–1981, 1992–1993, and 2000–2001. Only 2.7% of the 660 women at the 2000–2001 examination were taking lipid-lowering medications. After adjustment for age, education, diastolic blood pressure, body mass index, and smoking status, baseline cholesterol levels showed no relationship with subsequent development of dementia or Alzheimers. However, those who experienced the greatest decline in cholesterol levels over the 32-year follow up period also experienced far greater risk of dementia. A similar trend was seen for Alzheimer’s, but the results were not statistically significant.
So ... the research shows that people with high cholesterol levels are at lower risk of cognitive decline as they age.
Now, ask yourself: What group of people are most likely to be prescribed cholesterol-lowering drugs?
Exactly. People with high cholesterol - the same group of people who are at lower risk of cognitive decline in old age!
So what we are really seeing is the ability of statins to ride on the cognitive-protecting coat-tails of cholesterol - not a neuroprotective effect of statins themselves. As the RCT evidence shows, no such effect of statins exists. That evidence, in fact, shows just the opposite.
The relationship between statins and reduced dementia and Alzheimer’s is a misleading artifact of the relationship between high cholesterol and lower risk of cognitive decline.
This raises the possibility that the statin users in these epidemiological studies may have in fact experienced even better cognitive outcomes had they never taken neurotoxic statins.
Being Led Up the Statin Path
McCullough concludes: "In my view we can cross cognitive impairment or dementia off the list of concerns for statins as we use and take them to prevent heart attack, stroke, need for stenting or bypass surgery, and cardiac death."
I've written umpteen times previously, in detail, why the cholesterol theory is hogwash and why statins are a terrible choice for those wanting to lower their risk of heart disease and stroke. Suffice to say for now that the RCT evidence shows we cannot cross cognitive impairment or dementia off the list of concerns for statins.
McCullough's article finishes with the plea: "Please subscribe to Courageous Discourse as a paying or founder member so we can continue to bring you the truth."
But his article does not tell the truth; it spreads a dangerous falsehood.
The great irony of all this is that McCullough has made his name by rightly attacking a toxic group of gene therapies, a class of drugs that count neurological disorders among their most prevalent side effects. He is now praising another toxic class of drugs that count ... drum roll, please ... neurological disorders among their most prevalent side effects!
I never said the world makes sense.
After reading this, I wouldn't be at all surprised if McCullough goes and buys himself an Anthony Colpo voodoo doll and starts frantically sticking it with pins. Those things were huge sellers back in the hey-day of low-carb, I'm told (I hear they still occasionally pop up on vegan dark-web sites).
But the purpose of this article is not to belittle or demean Dr McCullough. I mean it when I say his efforts to highlight the dangers of the poison pricks are highly admirable.
His praise of the poison pills known as statins, however, is most regrettable. I don't believe he has any hidden or sinister agenda. I'm no telepathic psychoanalyst (unlike the rest of the internet, apparently), but it seems to me he may be succumbing to pressure, trying to prove to the mainstream he is not the quack they've vigorously made him out to be.
Dr McCullough has persisted with his activism despite being subjected to a heavy dose of cancel culture. At least two of his published articles have been retracted on dubious grounds, and when he announced a speaking tour of increasingly Orwellian Australia, the sexually deviant, Nazi wannabes that run the place wanted to ban him from entering the country. When that didn't happen, ticket outlet Eventbrite cancelled sales to his shows, forcing organizers to scramble for alternative arrangements. Eventbrite's excuse was that "the event does not comply with our Community Guidelines."
In 2022, he was stripped of his medical certifications, and in 2021 Baylor Scott & White Health tried to sue him for allegedly "spreading COVID-19 misinformation" under the Baylor name in media interviews (the ridiculous suit was eventually dismissed by a Dallas court in early 2023).
My advice to Dr McCullough, for what it's worth: If you're trying to appease the mainstream, forget it - it's a malevolent entity that has done you no favours. Just like the COVID gene therapies, statins are toxic garbage that should never have seen the light of day. Pretending otherwise is not being "balanced" and "fair" - it's being dangerously wrong.
I’d also encourage Dr McCullough to carefully read the comments section underneath his article, where surprised readers have shared their own often-debilitating neurological side effects from statin use.
---
Please subscribe to Anthony Colpo's Substack as a paying member so that I can continue to bring you the actual science, as opposed to myth and propaganda.





I agree - it IS disappointing to see him promoting a dangerous med. He figured out the vax dangers early on; why can't he see this?
Have to remember something tho. He IS a doctor and has therefore spent many years in the hallowed halls of brainwashing (med school). That's bound to come out somewhere.
Why take a Statin when many other natural substances work as well or better:
"What impact does niacin have on cholesterol?
Niacin can lower triglycerides by 25% and raise HDL cholesterol by more than 30%."
Apples & onions contain the flavonoid quercetin, as do many other fruits & vegetables. Apples also contain millions of beneficial bacterial, and pectin, both good for gut health. Thus, an apple a day can keep the doctor away, much to the chagrin of Big Pharma:
"Quercetin is one of the most common flavonoids. More and more studies have found that quercetin has great potential utilization value in cardiovascular diseases (CVD), such as antioxidant, antiplatelet aggregation, antibacterial, cholesterol lowering, endothelial cell protection, etc. However, the medicinal value of quercetin is mostly limited to animal models and preclinical studies.
"Test tube studies show that quercetin prevents damage from LDL cholesterol, and population studies show that people who eat diets high in flavonoids have lower cholesterol. One study found that people who took quercetin and an alcohol-free red wine extract (which contains quercetin) had less damage from LDL cholesterol. Another study found that quercetin reduced LDL concentrations in overweight subjects who were at high risk of heart disease."
Perhaps if 1% of the efforts poured into pushing Statins (or profits) were applied to studying quercetin and other natural flavonoids, we would know exactly how beneficial they are. A few studies on quercetin and cholesterol that I read were gamed by too low of a dose to be effective.
Firemen wear heat and flame proof clothing to protect themselves. Police military wear body armor. Cells also have protective sacrificial armor in the form of the antioxidant glutathione that prevents natural beneficial and excess oxidation from harming the cells. Once glutathione is depleted, cells are easily damaged and harmed, just as a naked firefighter would be quickly burned. It is nearly impossible for fully depleted glutathione to be restored with a normal diet, especially if a chronic cause of depletion is not eliminated. This leads to a chronic disease state, and a damaged cardiovascular system, which in turn leads to plaque building up like rust scale inside iron pipes. Our food supply is loaded with glyphosphates, which cause oxidative stress and damage to cells 24/7 as they flow through our vessels. The supplements NAC and methylfolate will both replete glutathione, and protect against glyphosphates. NAC ameliorates the toxic effects of glyphosphates. So why not take NAC instead of statins, and cholesterol levels will be of little or no consequence?
Because there's no profit for doctors or Big Pharma in NAC. Or quercetin or niacin. They do not cause side effects that require more prescription drugs in perpetuity to treat.
Dr. McCullough is a pill pushing allopathic doctor and defender of the same, yet he also sells supplements and knows full well their benefits. If there was an Olympic competition for the mind, he'd be a gold medalist. That he depends Statin drugs is indefensible, IMO
MAybe he needs to slow down once in a while, take some time off, and maybe he'd see things from a different perspective. The allegory of the tortoise and the hare applies to the practice of medicine as well as anything else.